Birth Story of Lucien
I wanted to go through Lucien's birth story 18 months postpartum and put a couple notes in here. I still struggle when I think back on his birth and over the last 18 months I have learned that my feelings a normal; it takes time to process and I am still working on that.
I don’t even know where to start – it was no secret that our babe was laying breech inside my belly. We had done just about everything we could to turn the baby but we did not have any luck. We were originally planning a homebirth with Nancy as our Midwife. Since finding out our baby was breech we started preparing for a Hospital birth at UNC.
I still remember the day we confirmed he was breech. It was New Years Eve. I cried. A lot. I had always envisioned welcoming my child into my arms surrounded by those we loved and cared about. Sure, it wasn't the end of the world if I delivered in a hospital; millions do it every year… but I was slowly losing control of my birth and that was the hardest part to accept.
Sunday night I got a phone call from Nancy. We had been seeing UNC Family Medicine for our parallel care and somehow it was not noted to my chart that we wanted a planned vaginal breech birth. Nancy planned to call and set up an appointment with a Doctor at UNC so that we could get my chart updated. We didn’t want to show up in labor and surprise them. Right before bed, I had a little pep talk with my baby bump. I told my bump that Mommy was done and uncomfortable and really needed him/her to come out and play! I said, “IF you are a boy and IF you come tomorrow I am going to name you Lucien.” It didn’t matter what Daddy thought – I was going to fight for this name! I fell in love with it back in August and had not been able to get it out of my mind. Sure enough… 5am I woke up to contractions at 5 minutes apart. They weren’t too strong – in fact I wasn’t even sure they were real. I figured they would taper off and go away. I had only slept 2 or 3 hours, so I imagined fatigue could have brought them on. I continued contracting for 2.5 hours and at 7:30am I called Nancy. She chuckled a little – of course this would happen! She had yet to call and make an appointment with the doctor since they weren’t open until 8am. So Nancy told me to go have breakfast and jump in the tub. The goal was to slow them down just a little.
It was a school day for my oldest, Michael. I remember him coming in the bathroom to give me a kiss before my husband took him to school. My heart ached knowing that he wouldn't witness the birth of his sibling, and I teared up knowing that was the last time I was going to kiss him as an only child.
Once in the tub they spaced out to about 7-8 min apart. We had an appointment at UNC at 11 but they wanted me to come in earlier for an NST. So we tried to get everything all packed up and ready to go.
There is a long walkway from the parking lot to the hospital. Well, it's not THAT long… but oh was it long on that Monday morning. Lucien was 5 months old when I made that walk again (heading in to photograph a birth). I parked the car and felt my breath escape me. Why?!? I wasn't here to give birth… but that walk… my whole birth flooded back to me in that moment. I gathered my bags and made it to the bridge way, inhaled, and with my heart in my throat I started walking. To this day I still take pause as I walk into that hospital.
We got to UNC around 10:45am and got started with our NST. Nancy had arrived, so she came back with us. The nurse hooked me up to the monitors and mentioned to me what they were – one measures the heartbeat, and the other monitor was measuring any contractions. Sure enough as we got started a contraction started to grow. The nurse asked if I felt that… I kind of chuckled and told her I had. Sure enough contractions were still coming every 5 min. After the 25 min strip she did a quick ultrasound. She was not able to locate any fluid pockets. We were supposed to meet with a doctor at 11am (and had blown right past that appointment – oops!). That doctor and another tech came in to take a second peek at the baby. She was unable to find fluid pockets as well. She confirmed baby to be frank breech. The doctor asked if we could go to another room to ‘chat’. It was quite funny, he started off telling me he understood I was a homebirth patient at first. He asked me what I imagined he would say. Of course my response was – knowing that they couldn’t find much fluid and the fact that I am contracting I figured he wasn’t going to let me go home. He smiled and agreed and then we all walked upstairs to L&D for admitting. They sent us to room #5. Normally this wouldn’t make it into the story… but when they told me this I was almost in tears. The number five is my son’s FAVORTIE number. It was a sign. This whole day so far was unfolding in such a way that kept me calm and I felt in control. Once to our room, our nurse hooked us up to the monitors. I was sitting in the bed working through the contractions and Dr. Smid came in to introduce herself and to talk about the plan we had in mind. Everyone was well aware that I came in with a lot of knowledge about breech birth so no one ever talked down to me. Rather, they asked what I knew and then they supplemented with anything I had missed. We discussed what to expect. I mentioned that with breech births, I was under the impression that one of two things is going to happen. I understood that this labor and birth would progress normally, I would dilate, baby would descend and baby would come out OR my labor could get hung up around the 7/8 cm mark and baby wouldn’t descend. She agreed. We also discussed what would happen once we go to the OR for the vaginal birth. I knew (or rather felt) that our baby was going to be a good hefty size. My 1st baby was 8lbs 10oz and I figured this one would be similar if not just over 9lbs. Dr. Smid was honest in saying that most of the breech births they do are Twin B – so the babies are much smaller. She mentioned that it had been a while since they had a breech birth of a baby this size. Naturally, this brought on some new conversations. Since this baby was going to be on the ‘larger side’ she said that once the body is out they will use forceps to help tuck the chin to the chest and help pull out the head; while at the same time someone will be pressing down on my stomach. This was done to avoid ‘head entrapment’. She also mentioned that as a last resort they may have to cut my cervix. WOAH! This was quite scary to think about. I understood it was a last resort but it really did set me back a little. Dr. Smid also mentioned that they recommend I get an epidural. This will lesson any resistance or tensing I may have during pushing which may delay the birth of my baby. Although I came prepared – this was a lot of information to take in all at once. I was doing my best to stay as composed and clear minded as I could but I was getting overwhelmed very quickly. Not to mention my contractions were now getting to a point where I couldn’t have a conversation through them. Dr. Smid asked if she could check me since things looked at though they were picking up; I obliged. I was at 5cm, negative 2 station.
In reading this back, and in learning more over the last 18 months. If I am faced with a breech delivery again I will forgo the use of forceps. Hands off baby is the route I would choose to take. I think this moment and this conversation was the turning point in my labor and the first seed of doubt that started to smolder. Knowledge is power, and if I had known these procedures beforehand I would have been prepared to respond and process.
Joe made the call to our birth photographer and doula to give them the update. They both started heading our way. This was happening… and I was the talk of the floor! The anesthesiologist came in to talk a little about an epidural. At this point I was undecided as far as if I wanted it. I am not going to lie – the thought of forceps, someone pushing on my stomach and possibly a cut cervix was wigging me out. The pain of contractions and pushing was not scaring me – I had done it before with my 1st so I knew I could do it. But I was nervous… so I did listen and ask questions about the epidural. I told him I was still unsure but that I wanted to make it as far as I could without one. In no way was I interested in slowing anything down and I wanted to be up and moving as much as possible while laboring. I also knew that in the event of an emergency – if I did not have the epidural they would have to put me under general, and I would be asleep for the birth of my baby. That also weighed in on my decision. So I signed all the paper work in case I decided to get one – but I declined it at that point and would call him in if/when I changed my mind. So next – in came the ‘team’ that would deliver me (if I happened to have a baby before 5pm). There were about 4 or 5 Doctors, Fellows and Residents. Just before they had come in I had sent Joe out to the car to go grab our labor bag. So it was just Nancy and I. They circled around my bed so that we could talk. (Not intimidating at all!)
I also remember not being able to see Nancy… she and been walled off. I felt small, weak and scared. I needed to feel empowered, comforted and supported. In that moment I struggled to stay present. I remember once it was over, I looked Nancy in the eyes and simply said "that was hard". She smiled and calmly replied that she was in awe of my strength and clarity. I appreciate her observation but I felt like I was losing control at a rapid rate.
They had brought in the paperwork that I needed to sign in order to proceed against their medical advice. Dr. Smid said, “Of course we recommend that you have a C-section – but if that is not your wish then we need to discuss the risks and you will have to sign this.” One of the other doctors chimed in asking me to repeat the risks of a vaginal breech birth to make sure I understood. I repeated back what Dr. Smid and I talked about; head entrapment. She prompted me with, “What else?” I responded, “Loss of oxygen.” She agreed, and then she placed her hand of my leg and said, “Your baby could die…I need you to repeat that to me…” Now I am still without Joe – and kind of panicking at this point. I took a deep breath and spoke the words that my baby may not survive. They then presented me with the forms and I signed them – all the while wondering if I was making the right decision. The instant the team left, Joe came back in and I broke down in tears doubting my abilities. Joe and Nancy both reminded me that I did have the courage to make the right decisions for THIS birth.
At this point it was about 2:30pm. Nancy had been with us the whole time so far. She was suggesting I get up and do some squatting. That of course DID NOT sound good – but she was right – and I knew it. I wanted this baby out and I wanted things to progress. So I did get out of bed and started squatting during the contractions. I leaned over the bed a little. I swayed my hips. Things were picking up. At about this time our birth photographer (Elizabeth) and our Doula (Brittany) arrived. Not being able to forget about thinking like a photographer, I put my skirt on so that my photos could be a bit more modest. Brittany and Joe were both there during every contraction, rubbing my arm, leg, back, and holding my hand. You name it and they were there! I thought to myself, “Of course I am having back labor! As if having a frank breech birth wasn’t enough – why not throw in some back labor?!” Brittany heated a rice sock to help with the pain. It did feel a bit better. My mother arrived at some point around 4pm. I really wish I had kept better track of time. But it really was all starting to blur together. Dr. Smid had come in to check me again. I was at 7cm, negative 2 station. Progress! I was leaning over the bed and during a very strong contraction I felt my water break. It was an odd feeling, but I was happy to know things were moving in the right direction. They placed a pad underneath me and they discovered meconium in the water. Going through my head, “Of course there would be meconium – frank breech presentation, back labor and now meconium.” And I kind of chuckled a little to myself. But I was still trying to rationally decide on whether or not I wanted the epidural. With meconium in the mix, my fear of something going wrong had now gone up. I know babies are born with meconium all the time – but my gut was now screaming at me that now was the time for the epidural.
My mother arrived at some point around 4pm. I really wish I had kept better track of time. But it really was all starting to blur together. Dr. Smid had come in to check me again. I was at 7cm, negative 2 station. Progress! I was leaning over the bed and during a very strong contraction I felt my water break. It was an odd feeling, but I was happy to know things were moving in the right direction. They placed a pad underneath me and they discovered meconium in the water. Going through my head, “Of course there would be meconium – frank breech presentation, back labor and now meconium.” And I kind of chuckled a little to myself. But I was still trying to rationally decide on whether or not I wanted the epidural. With meconium in the mix, my fear of something going wrong had now gone up. I know babies are born with meconium all the time – but my gut was now screaming at me that now was the time for the epidural. I noticed the clock, it was about 5pm and I knew there was a shift change about to happen so I put the call in to the anesthesiologist. He was in my room within 5 minutes. He figured he would sneak me in real quick before the change in shift. So they got me all set up, and everyone except Joe and Nancy were asked to leave the room. Before he started, I was sitting on the bed and had a strong contraction. With it, I could feel THICK meconium coming out. I couldn’t help saying, “OH MY GOD – I am shitting out of my VAGINA!” It made everyone laugh and kind of lightened the mood a little. The procedure was quick – thank goodness. It was not my proudest moment – I felt that people were going to judge me for getting the epidural.
I noticed the clock, it was about 5pm and I knew there was a shift change about to happen so I put the call in to the anesthesiologist. He was in my room within 5 minutes. He figured he would sneak me in real quick before the change in shift. So they got me all set up, and everyone except Joe and Nancy were asked to leave the room. Before he started, I was sitting on the bed and had a strong contraction. With it, I could feel THICK meconium coming out. I couldn’t help saying, “OH MY GOD – I am shitting out of my VAGINA!” It made everyone laugh and kind of lightened the mood a little. The procedure was quick – thank goodness. It was not my proudest moment – I felt that people were going to judge me for getting the epidural.
I have never felt judgement on my epidural - I wrote his birth story after all this was so new - each birth is so very different and I really wanted to be present for my child's birth. It was the right decision for me. I don't think I could have mentally continued this birth after hearing their 'standard procedures' for breech birth.
Once they finished, Dr. Smid checked me again – I was at 8cm, negative 2 station. A little progress. After about 30 minutes, it was clear that the epidural was only working on my left side. That was a very strange feeling – one whole side was numb and I could feel the whole contraction on just my right side. The anesthesiologist said he could try pulling the catheter out a little to see if we could get the medicine to flow onto the right side. So we tried that, but 30 minutes later it was evident that this epidural was not working. Our next option was to have it re-done. A new doctor had come on at this point so we had a whole new guy re-doing the epidural. Once he finished placing it they checked me again. At this point my ‘Birth Team’ had switched. So Dr. McPherson was the one who checked me. She also found me to be at 8cm, negative 2 station. It was about 7:30pm at this point.
The first nurse I had, Holly, I see her in the halls of UNC all the time. She is such a friendly face and I was so sad to have her shift end. We find time here and there to catch up each time I see her and she loves seeing photos of Lucien.
Dr. Strauss and Dr. McPherson came back in to have a discussion after my last cervical check. Dr. Strauss started off by telling me he understood that I was well researched and he respected that, so he figured we could have a frank conversation (no pun intended). I completely agreed; I had a feeling where this was going to go. He mentioned that he was knowledgeable about breech birth (which I knew – he was on the short list of doctors that I knew would be willing to attend a breech birth at UNC). He brought up a study that was done in Canada. A group of women set out to try and prove that vaginal breech birth was just as safe as a breech C-section birth. Dr. Strauss stated that there were certain parameters that the women in the study had to fall under in order to be considered for the vaginal breech birth. Dr Strauss said bluntly, “If you were a part of this study – you would no longer fall under their criteria to attempt a breech birth and you would be a part of the cesarean group.” The guideline he was referring to was the women must dilate at least .5cm every hour. I had been progressing nicely – but it was no secret that we were starting to slow down. Dr. Strauss said he was willing to let me go further if that was what I wanted, but he knew I was well informed in breech birth and he was confident I would make the right choice for me. I asked if I could have one more hour to see if the epidural would help me relax enough to push past this stall. He agreed to let me go another hour. This was when I told everyone (including Joe) to go get some dinner. I wanted to lay down and rest anyway and get a nap in if I could. At 9:30pm, Dr. McPherson came back in to check me. Sure enough, I was still at 8cm, negative 2 station. She left Joe and I to talk it through privately. I felt in my heart that I had done all that I could do and that I had given it my best shot. I felt that our baby had given me a sign, and I could not ignore this gut feeling that this was what needed to be done. I was scared, shaking, and part of me felt defeated – but I tried to stay in control, held Joe’s hand as we made the decision to have a C-section.
This was a surreal moment. I had so many thoughts flooding my mind. I failed. My body failed. I won't get to hold my slimy, wet, screaming baby right away. I would never have a home birth. My children will never see me give birth at home. I will forever have to fight for a VBAC… <--- that right there was the one that hurts the most
In our birth plan I wanted a ‘Gentle Cesarean.’ We talked with the doctors. We still didn’t know the gender so it was important for us to find out together – or have my husband announce it to me. I wanted delayed cord clamping. I wanted very much to have my baby on my chest right after birth. I asked if they could perform the routine procedures on my chest as well. I asked for them to double suture my uterus and told them I wanted to be sewn closed versus stapled. I asked to have my photographer in the room. I had my ‘polite pants’ on this whole time and simply told everyone that this was my job – I am a Birth Photographer. I let everyone know how important it was to me to have the photos of my husband and I meeting our baby for the first time. Everyone was on board – they even agreed to let Elizabeth in the room to photograph!! NICU was going to be in the room because of the meconium – so they also consented to let me have baby right away as long as baby was doing well. I was in agreement with them – my baby’s health was first and foremost. This was happening… I wasn’t going to get the natural homebirth of my dreams – but I was on my way to achieving the best possible cesarean with an amazing birth team behind me! It was about 10:00pm and it was time for me to say goodbye to everyone as they headed off to the waiting room. I remember Julie placing her hands on my belly and saying a little prayer. I fought back tears and kept repeating to myself that everything was going to be ok. So there we were… Joe, Elizabeth, and I alone in the room. They came to get me, unlocked my bed and started wheeling me out of the room and down the hall. Joe and Elizabeth stayed behind to get dressed in their scrubs. The only thing going through my mind was, “This is happening – I will be fine – baby will be fine.” Once in the operating room, they moved me to the table. Someone told me not to be nervous – they are like a NASCAR pit crew; they move really fast but knew what they were doing. I remember the anesthesiologist pumping drugs through my catheter. I slowly started to feel more and more numb. They strapped my legs down and laid my arms out to the side. They raised the table and then tilted it to the side. With the curtain set up, I could no longer see what they were doing down below my chest. They checked my numbness with a sharp poker and I was numb up to my armpits! The anesthesiologist then leaned in to tell me, “They JUST pinched your belly really, really hard with pinchers – and you didn’t flinch. I’d say you are numb!” Thank goodness I thought. I will admit I was nervous about being awake through this whole thing and afraid I would feel what was happening. But knowing that I was totally numb made me feel so much better.
Gosh reading through this… I am in tears. I find myself lying on that table reliving this. I held onto my Anesthesiologist's hand, I was shaking. I couldn't form words… I couldn't even get a coherent sound to roll off my tongue. It took a full minute for me to simply ask Joe... "talk to me"
Joe and Elizabeth finally walked in the room. It was about time. I was feeling quite overwhelmed and just needed my husband near me. I was shaking so much at this point. I am sure it had a lot to do with the medicine, but the adrenaline played a role as well. I was shaking so much I couldn’t form words. I remember holding not only Joe’s hand, but the anesthesiologist’s as well. They announced they were getting started and it all got so real. I needed a distraction to get my mind off this uncontrollable shaking. I asked Joe to just start talking – I prompted him to talk to me about our honeymoon. That morphed into him promising to take me there again! At some point Joe told me – OK you win! You can name the baby what you promised last night if it’s a boy. I still had yet to tell him what that name was – so I took that moment to tell him I had called him Lucien. I heard the doctor say they were at the uterus. OK this is it – I was going to meet my baby any minute… I was going to see my baby’s face over the curtain any second now… I then heard the doctor say… “OK we are delaying the clamping of the cord. We are cutting the cord. Mom – we need to send baby over to see NICU first.” My mind was racing… but nothing had really sunk in just yet. They did not lift baby over the curtain… I still didn’t have a visual to hold onto. The NICU Doctor did say Joe could come over to see the gender. I remember him standing and walking over, taking a peak and coming back to tell me that we have a Lucien Christopher. I knew it was a boy! Then I overheard that his APGAR was only a 1. Joe had put on a pretty good poker face because he told me after the fact that he was internally freaking out. I kept repeating out loud – “I knew it was a boy, I knew it!” I was trying to keep my mind off the fact that I couldn’t hear him crying…
My mind was racing… but nothing had really sunk in just yet. They did not lift baby over the curtain… I still didn’t have a visual to hold onto. The NICU Doctor did say Joe could come over to see the gender. I remember him standing and walking over, taking a peak and coming back to tell me that we have a Lucien Christopher. I knew it was a boy! Then I overheard that his APGAR was only a 1. Joe had put on a pretty good poker face because he told me after the fact that he was internally freaking out. I kept repeating out loud – “I knew it was a boy, I knew it!” I was trying to keep my mind off the fact that I couldn’t hear him crying… Then about 4 or 5 minutes after he was born we heard his first cry. They brought him right over to me and laid him on my chest, skin to skin. They had placed the hat that I had made him on his head and there he was – staring right into my eyes. I had very little feeling in my arms and hands so Joe literally held him on my chest. I was able to stroke his forehead with my thumb, a feeling he had felt in utero for the last month! I kissed him; his skin was so soft, his body so warm, his hands so wrinkly…
Then about 4 or 5 minutes after he was born we heard his first cry. They brought him right over to me and laid him on my chest, skin to skin. They had placed the hat that I had made him on his head and there he was – staring right into my eyes. I had very little feeling in my arms and hands so Joe literally held him on my chest. I was able to stroke his forehead with my thumb, a feeling he had felt in utero for the last month! I kissed him; his skin was so soft, his body so warm, his hands so wrinkly… After about 15 minutes I was getting really tired so I asked that Joe hold him. Of course he was happy to do so. When they had finished closing me, they moved us to recovery. Once my wheels were locked, they sat me up a little and handed him back to me. I worked to latch him on and he did - right away! It was such a different experience from my first son! He was content and nursed for about 30 minutes while Joe and I just admired him. It was close to midnight, so I sent Joe and Elizabeth out to go tell everyone HE was here. Everyone was waiting in the waiting room anxiously… Elizabeth got pictures of my Mom’s reaction to learning she has a new grandson. (Another reason why I am thankful to have my birth photographer there; she was able to capture the moments I could not see).
After about 15 minutes I was getting really tired so I asked that Joe hold him. Of course he was happy to do so. When they had finished closing me, they moved us to recovery. Once my wheels were locked, they sat me up a little and handed him back to me. I worked to latch him on and he did - right away! It was such a different experience from my first son! He was content and nursed for about 30 minutes while Joe and I just admired him. It was close to midnight, so I sent Joe and Elizabeth out to go tell everyone HE was here. Everyone was waiting in the waiting room anxiously… Elizabeth got pictures of my Mom’s reaction to learning she has a new grandson. (Another reason why I am thankful to have my birth photographer there; she was able to capture the moments I could not see).
 I had a steady stream of visitors back to my recovery room. Everyone was anxious to meet Lucien. Around 2am we were taken to our postpartum room. One of Nancy’s Birth Assistants is a nurse at UNC and we were assigned to her room that night. It was so wonderful to have a familiar face that evening and into the morning.
I had a steady stream of visitors back to my recovery room. Everyone was anxious to meet Lucien. Around 2am we were taken to our postpartum room. One of Nancy’s Birth Assistants is a nurse at UNC and we were assigned to her room that night. It was so wonderful to have a familiar face that evening and into the morning.
Belinda - she was a little slice of home in the midst of chaos for me. Her smile brightened my room at 2am. Her presence that night (and our last night) was the best part about our UNC stay.
 This was definitely not the route that we had envisioned this birth going. But as it turns out it was what NEEDED to happen.
This was definitely not the route that we had envisioned this birth going. But as it turns out it was what NEEDED to happen.
So I added that part up there to my birth story because I felt obligated… like I NEEDED a reason to feel OK with how things went. But you know what, I still struggle. Sure this was the best and safest way for him to come into this world, but that DOES NOT make it any easier to accept. Yes of course a healthy baby and healthy mama are important, but damn! I missed out on the birth of my dreams. My son was born under bright operating room lights, the first person he laid eyes on was not his mom or dad, the first touch he felt was not that of love or gentleness - this was not the start I had envisioned for him. Birth transforms us, and I still struggle to find the space to accept how Lucien was born into this world. I still get weak in the knees when I walk into the operating room to photograph a cesarean. My mind flashes to a time in my life where I laid strapped to a table, exposed... and I felt out of control, weak, and vulnerable, yet I still felt empowered. Contradicting feelings I know, but I am so thankful for that ounce of empowerment because without it I would not be the person I am today.
On the third or fourth day after his birth, we got a call from our placenta encapsulator. She noticed there was an abnormality with our placenta called Vasa Previa. It is a very rare condition where one or more of the veins are unsupported by the umbilical cord or placenta tissue. It carries a high mortality rate because it is rarely tested for and detected. If the membranes rupture across the unsupported vessel, the result is death within 2-3 minutes due to blood loss. Those that have a known diagnosis of Vasa Previa are hospitalized and put on bed rest during their 3rd trimester and have baby via cesarean at 35 weeks. This is done at that time, because it is late enough that the baby has a good chance of living; but early enough that the chance of water breaking is low. Now that I know all of this information – I understand we are truly very lucky. Our little man KNEW exactly what to do to warn us. He was laying breech as a way of telling us that we needed to be in the hospital and that a c-section was a necessity. When we found this all out – I was sick to my stomach. He had been in my life for 4 days at this point and I couldn’t even imagine not having him with us. Thinking back – we had TWO versions done! That was so dangerous. My water broke and we were so lucky that the blood vessel was not compromised. He definitely had a guardian angel – maybe more than one. He was meant to be in this world…
Time will heal, I do believe this. He latched with no issues, and from that moment we developed a bond that will never be broken. He recognized my voice, and his favorite spot to lay was on my chest. My heartbeat so familiar to him; for so long he sat with is head in my ribs, so close to my heart. I know that he loves me despite how he was born.I am strong, I can do hard things, I can.
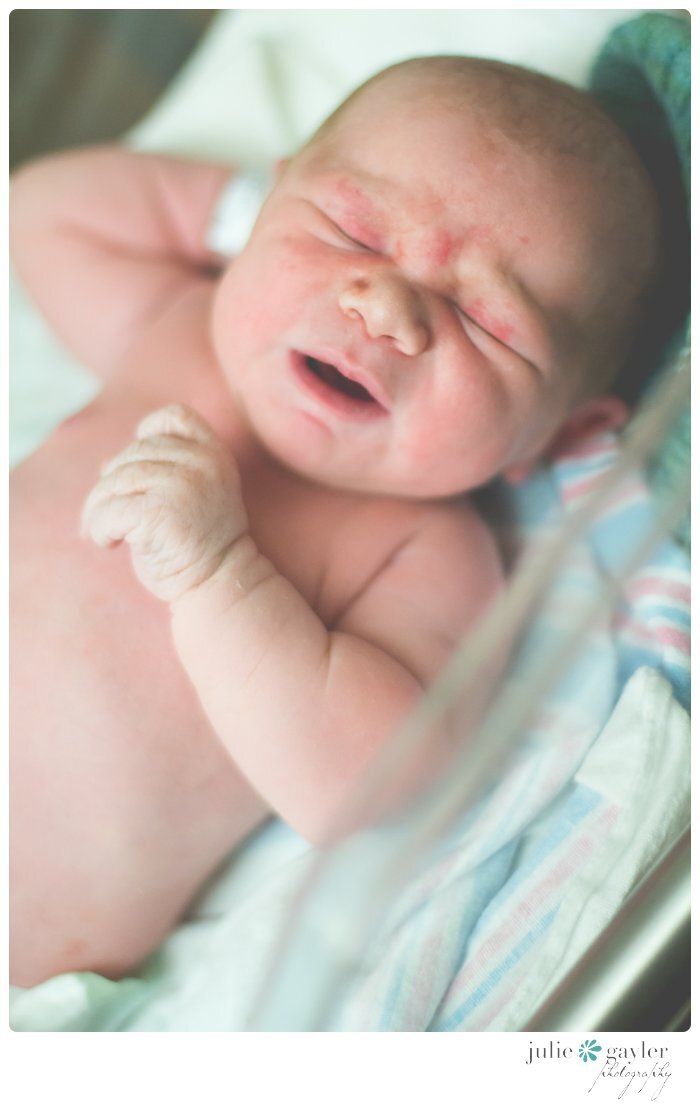
Lucien Christopher
February 3rd 2014
10:45pm
9 pounds 4 ounces
20.5 inches long
.
.
.
**THANK YOU so much to**
Elizabeth of Ruby Laine Photography
Julie of Julie Gayler Photography
Brittany of Peaceful Path Birthing
Nancy of Birthwise of Central NC